The Future of Medicine: Electroceuticals
by Scott Dutfield · 01/08/2019

Should we ditch drugs to make way for an electrical alternative?
A great many of us often don’t think twice about popping a pill to treat a chronic condition. The most up-to-date data from the European Union suggests around 49 per cent of people within its 28-member countries aged 15 and over use prescribed medicines. However, with the introduction and development of bioelectronic technologies, pills could soon be a thing of the past for some conditions.
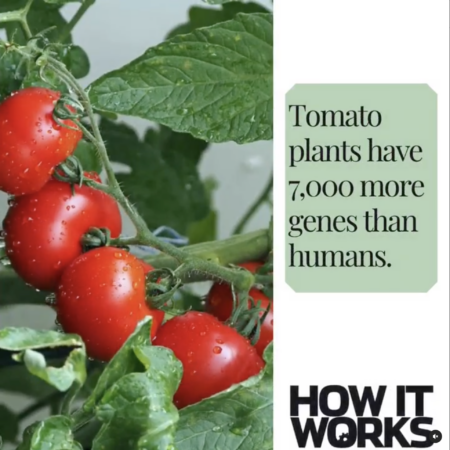
Implanted electrical devices that work to repair, replace or restore parts of our bodies have been employed by doctors since the 1950s. The first cardiac pacemaker was implanted in a 43-year-old male back in 1958 to combat his cardiac arrhythmia. Since then devices have been created to restore senses such as hearing and sight and regulate insulin for those suffering from diabetes. However, in recent years ‘electroceutical’ devices have been making waves as a treatment for chronic conditions.
Fundamentally, the principle of electroceuticals is to emit a low-energy electrical pulse to stimulate different nerves in the body to aid the reduction of symptoms for an array of physical conditions such as epilepsy and rheumatoid arthritis. Recent investigations into externally worn devices have even suggested that they might be a treatment solution for mental health conditions such as depression and anxiety, an incredibly exciting possibility.
One of the biggest downfalls of chemical medication are the potential side-effects they can cause. These side-effects mostly occur due to pharmaceuticals affecting not only the intended target but several organs when they enter the body. Electroceutical treatments offer a more accurate approach as they can focus on
particular nerves connected to specific organs, limiting the number of side-effects. For example, one of the most widespread uses of electroceuticals is treating epilepsy with a vagus nerve stimulation (VNS) device. Epilepsy is a condition whereby nerves ‘fire off’ abnormally when sending signals to different parts of the body, resulting in seizures of varying degrees. The condition affects more than 500,000 people in the UK alone. VNS devices are able to help manage these symptoms through artificial electrical stimulation.
Implanted beneath the skin and hooked onto the vagus nerve at the neck, a generator, which resembles that of a pacemaker, creates electrical pulses that feed through a lead to the nerve at regular intervals. This stimulation regulates the electrical signals through the vagus nerve into the brain, reducing seizures. Should a seizure occur, or even a warning of an oncoming episode, a handheld magnet can be waved over the implant’s generator to produce more impulses, preventing or reducing its longevity.
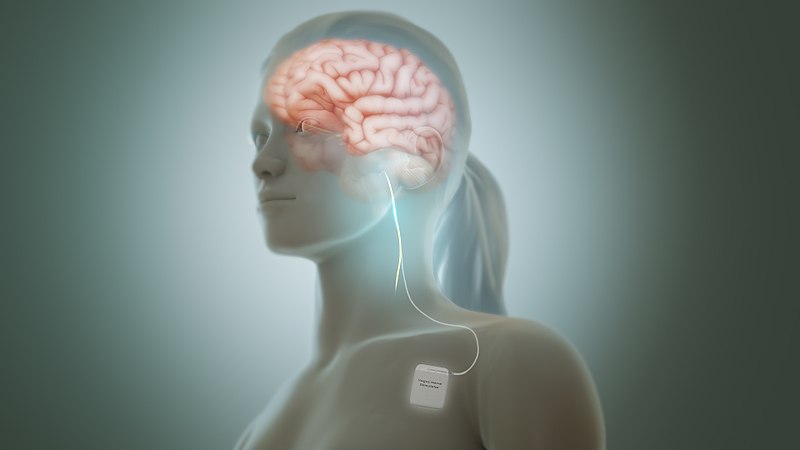 Vagus nerve stimulator (VNS) devices are implanted under the skin to treat epilepsy Credit: Scientific Animations
Vagus nerve stimulator (VNS) devices are implanted under the skin to treat epilepsy Credit: Scientific Animations
In order to use nerves as a method of treatment, scientists must first locate which nerve carries which message and to where around the body. Brain mapping is a way of creating a road map of the mind to reveal all the avenues through the body. There are several methods currently used to map the brain, one of which is electromyography, which measures the electrical activity in the brain through electrodes placed around the head. However, each of our brains is wired differently, with the exception of major nerves such as the vagus nerve. Therefore it is difficult to create universal electroceuticals, and thus far a complete map of the brain’s complex network of neurons is yet to be visualised.
Though VNS devices seem to hold the monopoly on bioelectronics, recent discoveries are shedding light on the potential for electroceuticals to repair physical damage within the body too. Earlier this year researchers at the Northwestern University and the University of Washington, US, created an implantable wireless device that speeds up the regeneration of damaged nerves.
The device (trialled on rats) emits regular pulses of electricity to damaged sciatic nerves to accelerate nerve growth and enhance muscle control and recovery. Consisting of a thin disc that wraps around nerves, the stimulator is activated wirelessly by a transmitter outside the body. This technology is designed to only work for a specific amount of time during the healing process. Engineers use materials that allow it to biodegrade and be absorbed into the body, preventing another extraction surgery.
Of course, electroceuticals are not the answer to all of our medical problems; bacterial diseases, for example, cannot be treated using these electrifying methods. Electroceutical technology is still in its medical infancy in terms of its general use, and its long-term effects have yet to be determined.
Meet the man behind Modius – the electro-stimulation headset that tricks the brain into thinking you’re working out
This article was originally published in How It Works issue 120
For more science and technology articles, pick up the latest copy of How It Works from all good retailers or from our website now. If you have a tablet or smartphone, you can also download the digital version onto your iOS or Android device. To make sure you never miss an issue of How It Works magazine, subscribe today!