Bacteria: the good, the bad, and the ugly
by How It Works Team · 17/09/2019
Your body is home to trillions of microbes, and you wouldn’t survive without them.
It might surprise you to know that only around half the cells that make up your body are actually human. The average person has an estimated one-to-one ratio of human cells to microbes, the majority of which are bacteria. Known as the microbiome, your body’s bacterial ecosystem has a huge influence on your health.
Bacteria often get a bad rap. Some of them cause infections, make you feel sick, and a few even appear to feast on your flesh. That said,
these harmful germs are in the minority.
Fewer than five per cent of microbes are known to cause disease in humans and the majority of bacteria that call your body home are harmless.
Many species, particularly those that reside in our digestive systems, are highly beneficial. Researchers are only just starting to discover the extent to which gut bacteria influence our health. The bacteria that colonise your intestines (known as gut flora) help break down some of the foods that you can’t digest into nutrients that you can. They also produce some vitamins that your body can’t synthesise on its own, including K2 (which helps blood clot properly) and B12 (involved in several key functions, including protein metabolism). The overwhelming presence of good bacteria in a healthy gut helps suppress the growth and survival of bad bacteria, protecting us from illness.
The role of your intestinal bacteria extends far beyond digestion. Studies have linked imbalances in gut flora to a range of conditions, including heart disease, diabetes, colic and Parkinson’s. The health and diversity of your microbiome can influence how effective your immune system is, and can even affect your behaviour and mental health.
Research suggests that the combination of different bacteria in your gut is an important factor in whether or not you become obese or develop diabetes. The composition of your microbiome can change how you store fat,
how you regulate blood glucose levels and how your body responds to the hormones that regulate appetite. Obese individuals tend to
have a less diverse microbiome, whereas the gut flora of lean people includes a wide variety of bacterial species.
Although the majority of your body’s bacteria resides in your intestines, your skin also plays host to a multitude of microbes. Your skin flora helps regulate inflammation, a process that helps the body heal but can be damaging if left unchecked. Research by the University of Oregon found that we are each surrounded by our own personal atmosphere of microbes. Your microbiome is unique like a fingerprint: it is even possible to identify someone from a sample of their bacterial ‘cloud’.
Prebiotics and probiotics
Diet is a very significant factor in the health of your gut flora. Both prebiotic and probiotic foods are beneficial to your microbiome, but what is the difference between the two?
Probiotic foods contain live bacteria that give your digestive system a helping hand. Foods that are made through fermentation – a process by which bacteria naturally present in the food start digesting its sugars – are rich in probiotics. This group includes yoghurt, sauerkraut, kimchi and some cheeses.
Prebiotic foods are also high in certain kinds of fibre, which we are unable to digest, but are a valuable source of nutrition for the bacteria in our guts. While all prebiotics are fibres, not all fibres are prebiotic; many vegetables, legumes, grains and nuts are naturally high in the types of fibre that keep gut bacteria healthy.
The bad and the ugly
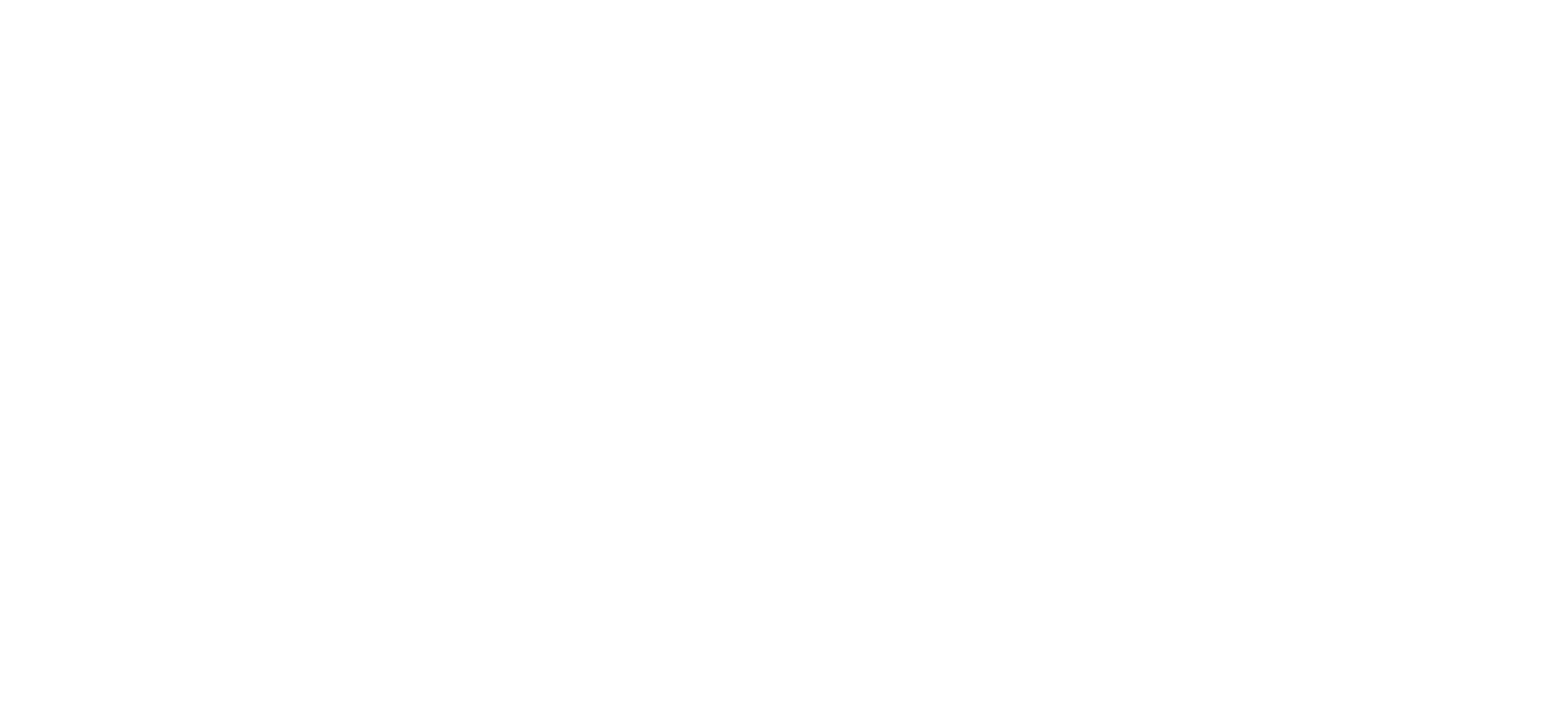
Although only a small fraction of known bacterial species causes disease, they are capable of wreaking havoc on our bodies. Harmful bacteria can enter the body in several ways. For instance, we can inhale or ingest them, or they can enter through broken skin.
Once inside, they can reach their target site, such as the lungs or intestines, where they attach to our cells and multiply. Our bodies provide these bacteria with nutrients, but in return they release toxins, which can damage our tissues.
Our immune system provides some protection against these microscopic invaders. Immune cells can identify and destroy pathogens, but some bacteria have evolved methods of evading our internal defence mechanisms. It is in cases where these hardy germs persist that we need the help of antibiotics to eliminate infections before they spread.
Bacteria adapt to their environment so quickly that if any survive, they can develop immunity to these medications. The rise of antibiotic-resistant ‘superbugs’, which can cause life-threatening infections, is an increasingly serious threat to global health.
Deadly bacteria
The most dangerous bugs spread easily, cause devastating illness, resist antibiotics, or are a lethal combination of all three
Group A Streptococcus
Infections from this bug are usually mild, but in rare cases they cause necrotising fasciitis, or ‘flesh-eating’ infections. The bacteria infect body tissues and produce toxins that destroy them.
Staphylococcus aureus
Superbug strains of these bacteria, known as MRSA, spread easily by human contact and have been a serious problem in hospitals. They can cause deadly diseases such as pneumonia.
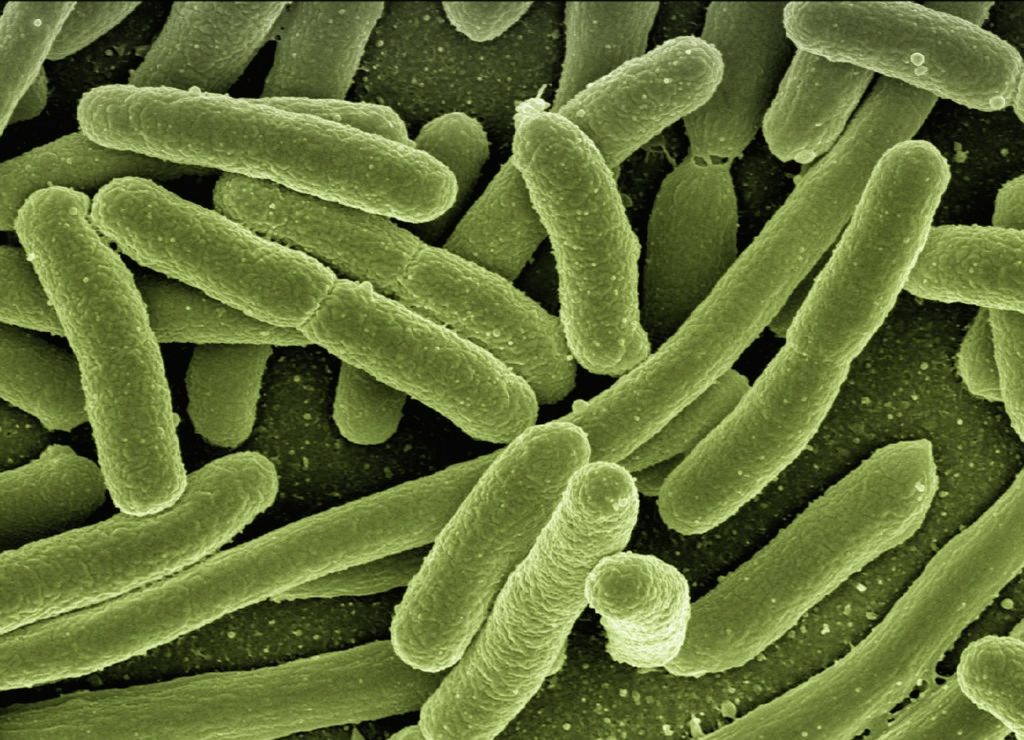
Escherichia coli
While most E. coli live
harmlessly in the gut, some strains can cause food poisoning or more severe problems, and have developed resistance to many antibiotics.Yersinia pestis
This bacterium was responsible for bubonic plague, or the Black Death, which caused millions of fatalities in the 14th century. Without treatment, it kills nearly 100 per cent of those infected.
This article was originally published in How It Works issue 88
For more science and technology articles, pick up the latest copy of How It Works from all good retailers or from our website now. If you have a tablet or smartphone, you can also download the digital version onto your iOS or Android device. To make sure you never miss an issue of How It Works magazine, subscribe today!